CPD Updates for GPs
2019 CPD Events
Barossa Valley
In September we held a peri-urban CPD event at the Novotel Barossa Valley in addition to the seminar held at Hahndorf in August. The category 2 CPD seminar was titled ‘Pregnancy Diagnosed – What’s Next? & All you need to know about Vaccinations, Supplements, Medications & Lifestyle in Pregnancy’ and was presented by Dr Jenni Goold.
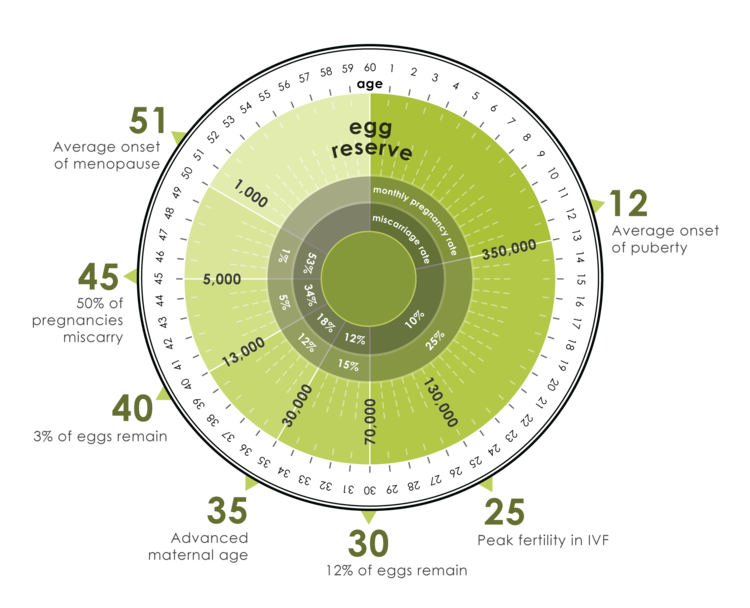
Dr Bruno Radesic, Consultant Gynaecologist and Fertility Specialist was invited and he gave an interesting presentation about Fertility Management.
Take home messages included the following:
- Up to 80% of couples conceive within 12 months
- 30% male, 30% female, 30% combo, 10% unexplained
- Infertile (azoospermia, blocked tubes) vs. Sub fertile (endometriosis)
- Preconception care critical
- Lifestyle 3/12 prior, changes non-coding DNA, with potential life-long health effects
- BMI, diet, exercise, smoking, ETOH, caffeine, stress – all important discussions
- Age matters!
When to refer to a Specialist:
- Age < 35 + trying to conceive > 12 months
- Age < 35 + trying to conceive >6 months + endometriosis, PCOS, gynaecological problems (past abdominal/pelvic surgery, PID etc.)
- Age >= 35 + trying to conceive > 6 months
- Special circumstances
- Advanced maternal age, recurrent miscarriage, sterilization, prior hx chemo/radiotherapy etc.
Accreditation Seminar
The GP Obstetric Shared Accreditation Seminar was repeated at the Adelaide Pavilion on Saturday 19th October and at the Adelaide Hills Convention Centre on Friday 22nd November to allow GPs to fulfil the mandatory requirement of attending at least one Accreditation Seminar in the triennium.
We were absolutely delighted with the number of GPs that attended on both days and we were treated to a range of relevant topics and excellent speakers. We were appreciative of the many emails we received expressing thanks for such informative, educational and enjoyable days.
An important take home message is that our Obstetric Shared Care program is based on the PPGs (South Australian Perinatal Practice Guidelines). They can be downloaded from our GPEx website or from the internet.
We are currently well underway updating the South Australian GP Shared Care Protocols and anticipate that distribution will be early 2020.
GPEx – ‘A Day in General Practice’
The GP Obstetric Shared Care Program has collaborated with GPEx again this year and has participated in a series of workshops designed for Registrars. The aim is to offer the Registrars an insight into becoming an Accredited Obstetric Shared Care GP provider and how to manage that first ante-natal consultation.
All four workshops have now been completed with a total of 133 Registrars attending.
We have been absolutely delighted with the positive feedback and even more so with the many enquires and new applications we have received.



GP Advisors:
We know that Michelle Emmerson delivered her son Troy on the 5th of August.
The family is doing very well and already Troy has been to two GP OSC CPD events as well as watched his Mum present at a GPEx workshop! Perhaps he will be a future OSC GP or Obstetrician!
What has Jenni Goold been up to?
Jenni has worked for over a decade in the Obstetric Antenatal Outpatients Department at the QEH, the LMcEHS and now the Women’s and Children’s Hospital as a Visiting Medical Officer.
Jenni was involved with the development of the SA GP Obstetric Shared Care Program in the mid 90’s and with the growth of the program and establishment of the statewide program as we now know it today. She is enthusiastic and passionate about Obstetric Shared Care and loves being involved in what she believes is a fantastic program for women and GPs.
In addition to these roles Jenni consults at Firle Medical Centre.
She is a Lactation Consultant and she now represents GP Obstetric Shared Care on the RANZCOG National Committee.
Thanks to Diplomate support, Jenni was elected to the RANZCOG GP Obstetric Advisory Committee as a Shared Care Representative for a term of 3 years recently. She feels that this is a very exciting opportunity to work closely with other colleagues from around Australia and New Zealand.
The GPOAC membership is comprised of:
- Dr Judith Gardiner Chair | Intrapartum Care Representative
- Dr Mark Farrugia Deputy Chair | Intrapartum Care Representative
- Dr Jennifer Goold | Shared Care Representative
- Dr Alison Green | Intrapartum Care Representative
- Dr Julia Marcello | Shared Care Representative
- Dr Vijay Roach | RANZCOG President – Ex-officio (Voting)
- Ms Vase Jovanoska | RANZCOG CEO
The GPOAC is focused on Diplomates, those in training and upskilling opportunities. The committee is looking for input from Diplomates, perhaps those recently graduated, to see how training can be improved and supported. Please let Jenni know if this is you. The GPOAC is also involved in organising the Diplomate Days at RANZCOG ASM, the next being in Hobart in 2020.
In addition, Jenni serves on the ethics and Standards committee of RANZCOG. She is also a member of the SA perinatal mortality Subcommittee. She has a Diploma in O&G, and a Diploma in Clinical Education which is another of her passions.
Please contact Jenni via Leanne at GP Partners for further information, assistance or feedback to these committees.
She also has four children and we think it is amazing how she juggles her time! Well done Jenni!
Our GP Advisors are present at all our GP OSC CPD Seminars.
Sharing Updates to the SA GP Obstetric Shared Care Protocols
Important! Change to the timing of Pertussis Immunisation in Pregnancy
The Australian Immunisation Guidelines and State Health Department protocols have been updated to recommend women be immunised from 20-32 weeks gestation, rather than from 28 weeks. Women can continue to receive a funded vaccine up until birth; however it takes 2 weeks for antibodies to peak, hence the recommendation for earlier immunisation.
The reasons for the change are simple:
- It provides for protection of premature babies
- There is evidence of similar antibody levels in cord blood from 2nd and 3rd trimester vaccination, with perhaps even higher levels from the 2nd trimester immunisation. Although there is lower transfer initially, there is a longer time to transfer, with the most efficient transfer being from 30 weeks gestation
- The research says it is safe for both mum and bub
- We will now have a broader target to hit.
For simplicity’s sake, we suggest that we change our practice and immunise women when we review their morphology scan. If a woman has received pertussis immunisation before 20 weeks, it does not have to be repeated in the current pregnancy. The data shows transfer of antibodies as early as 13 weeks.
The influenza vaccine, as we would all know, can be administered at any gestation and provides additional protection for the first six months of an infant’s life.
Click here for more information.
Vitamin D Status in Pregnancy
Routine Vitamin D supplementation for all women is now recommended.
Supplementation of infants at risk based on the post-natal maternal serum Vitamin D level recommended.
Chlamydia Screening
Screening for Chlamydia is recommended for all women under the age of 25 years.
A reminder about the changes with regard to gestational diabetes and overt diabetes and a reminder to arrange an early GTT for women at risk between 12 and 16 weeks ideally.
Click here for more information.
First Trimester Screening
A reminder that nuchal translucency greater than 3.5 is now considered abnormal rather than 3.0.
Mental Health
The Women’s and Children’s Hospital has implemented a screening tool for mental health referrals and many women who are struggling will now not meet this criteria. Consequently women will now be referred back to their GPs for their guidance and for completion of Mental Health Plans.
A number of Guidelines have been published on both the SA Health website (available at www.sahealth.sa.gov.au/perinatal and www.sahealth.sa.gov.au/neonatal) and web-based app (available at https://extapps.health.sa.gov.au/PracticeGuidelines). Please find attached the guideline upload summaries that detail key points/changes and risk management and/or budget implications.
Please review the summaries in detail to identify any implications for your area(s).
| September Summary of SA Health Neonatal Medication Guideline Updates SA PPG Upload to SA Health Website and Practice Guidelines Web-Based App |
We are Excited!
Now Available on our Website – Shared Care Podcasts
We are excited to announce that we have recorded a further Shared Care Podcast with Associate Professor Chris Barnett.
A/Prof Barnett has dual fellowships in neonatal/perinatal medicine and clinical genetics and is the head of the Paediatric and Reproductive Genetics Unit at the Women’s and Children’s Hospital in Adelaide. He is the clinical lead of the NHMRC funded Genomic Autopsy Project and on the expert advisory committee of the Genomics Health Futures Mission, the Australian government’s $500 million research investment in the future of genomic medicine in Australia. A/Prof Barnett’s neonatal training was done in Adelaide at the University of Adelaide and Women’s and Children’s Hospital and in Toronto, Canada at the University of Toronto and The Hospital for Sick Children.
He was a consultant neonatologist at the Women’s and Children’s Hospital from 1997-2002 and then in private neonatal/paediatric practice from 2002-2007. A/Prof Barnett is a past president of the SA branch of the Perinatal Society of Australia and New Zealand (PSANZ). A/Prof Barnett’s clinical genetics training was undertaken at University of Toronto and The Hospital for Sick Children, Toronto and at the Women’s and Children’s Hospital in Adelaide. He has research interests in prenatal genetics, fetal pathology and rare childhood diseases and has over 80 publications in peer-reviewed journals and has written multiple book chapters.
He talks with host GP Advisor Dr Annie Lin about the very topical Pre-Pregnancy Genetic Screening.
This podcast is now available via our GPEx website. Click here.
Our earlier podcast featuring Associate Professor David Ross is also available via the GP Partners website.
Excerpts:
Clinical Infectious Diseases, ciz429, https://doi.org/10.1093/cid/ciz429 Published: 24 August 2019 Abstract Background We evaluated the risk of pelvic inflammatory disease (PID), ectopic pregnancy, and infertility in women with a previous Chlamydia trachomatis (CT) diagnosis compared with women who tested negative for CT and CT untested … Continue reading →
Read on »
Changes to the National Cervical Screening Program (NCSP) Clinical Guidelines (2016)
Click Here
We wish to inform you of recent changes to the 2016 National Cervical Screening Program: Guidelines for the management of screen-detected abnormalities, screening in specific populations and investigation of abnormal vaginal bleeding (the Guidelines).
These Guidelines aim to provide guidance to health care professionals and women regarding current best practice in the clinical management of women with positive oncogenic HPV test results and abnormalities detected on subsequent liquid based cytology (LBC).
The National Cervical Screening Program Clinical Expert Panel has undertaken a review of the Guidelines in relation to a number of key issues raised by health care professionals. As such, a number of changes to the Guidelines have been implemented.
These changes are outlined below.
Chapter 18: Signs and symptoms of cervical cancer – identification and investigation of abnormal bleeding
he title for Chapter 18 has been changed to reflect the addition of a new subpage, Investigations of other symptoms – vaginal discharge and deep dyspareunia which provides detailed guidance for healthcare professionals on the identification of the signs and symptoms of cervical cancer.
Three new recommendations in relation to deep dyspareunia and unexplained persistent unusual vaginal discharge have also been added to the Guidelines. The new recommendations are:
- REC18.8 Women with abnormal vaginal discharge and/or deep dyspareunia: Almost all women with vaginal discharge and/or deep dyspareunia have benign gynaecological disease. They should be investigated appropriately and if due for cervical screening a routine CST would be the most appropriate test.
- REC18.9 Women with unexplained persistent unusual vaginal discharge: Women of any age with unexplained persistent unusual vaginal discharge, especially if offensive or blood stained) should be investigated with a co-test (HPV and LBC) and referred for gynaecological assessment.
- REC18.10 Women with unexplained persistent deep dyspareunia: Women with unexplained persistent deep dyspareunia in the absence of bleeding or discharge should have a CST if due and referral for gynaecological assessment should be considered.
Chapter 14: Screening in Pregnancy
The recommendations for screening in pregnancy in Chapter 14 have been modified to reflect expert opinion on the risks and benefits of self-collection of specimens for HPV testing during pregnancy. The previous recommendation stated that self-collection for HPV testing during pregnancy is not recommended.
The new recommendation is:
REC14.13 Self-collection in pregnancy: Self-collection for HPV testing may be considered during pregnancy in never-screened or under-screened women, following counselling by a health care professional regarding the risk of bleeding.
The Stillbirth CRE is working on a Safer Baby Bundle, which includes developing an education program for health professionals to reduce the stillbirth rate by focusing on five key areas.
As GPs, we can all get involved and help to reduce the trauma of stillbirth by:
- Assisting women and their families to quit smoking
- Appropriate referral if there are concerns about fetal growth
- Providing information about the importance of taking prompt action reduced fetal movements are detected
- Providing advice to go to sleep on their side, not their back, with the reassurance that, if they wake up on their back, don’t panic, just roll over and go back to sleep
- Being informed and supporting our colleagues when they are advising about the timing of birth.
On 15 October 2019 the Safer Baby Bundle launched eLearning resources to support healthcare professionals with new strategies to help reduce stillbirths.
The Stillbirth CRE in conjunction with the International Stillbirth Alliance (ISA) and the International Society for the Study and Prevention of Perinatal and Infant Death (ISPID) are presenting the 2020 International Conference on Stillbirth, Neonatal Death and Sudden Unexpected Death in Infancy (SUDI) in Brisbane next year.
The theme of the conference is ‘Drivers for global change’. It aims to showcase strategies to effectively address the burden of stillbirth, neonatal death and SUDI across high, middle and low-income country settings. You can subscribe to the Stillbirth CRE newsletter for conference updates.
Academy of Breastfeeding Medicine
Friday 1st May – Sunday 3rd May 2020

Baby Seats – CLICK HERE for details for your patients (PDF)
To provide Obstetric Shared Care in South Australia over 20 weeks, GPs must be accredited to the GP Obstetric Shared Care program.
CLICK HERE to download an application form to join the program
CLICK HERE to order the latest version of the SA Pregnancy Record – Version 11
If you have any queries concerning the GP Obstetric Shared Care Program please contact Leanne March, GP Shared Care Programs Manager at GPEx:
Leanne.March@gpex.com.au
We are listening to your feedback…
In 2020 we will be continuing to offer you CPD Events, Podcasts and Webinars with greater relevance and interactive opportunities!
All CPD events with GPEx are free of charge and accredited with RACGP and ACRRM
Looking forward to seeing you next year!
Please Update your Details
It is important and a mandatory requirement to maintain your accreditation that you advise the Program of your current up-to-date details.
Please contact Leanne, Obstetric Shared Care Program Manager if your details have changed or you can click on the link below to complete an up-date form.
Forms can be emailed to Leanne.March@gpex.com.au