How are your motivational interviewing skills?

How are your skills in motivational interviewing? Brush up on this important skill for the RACGP CCE.
Have you ever had a patient struggle to make lifestyle changes to improve their chronic condition or health in general? GPs must not only apply multiple clinical guidelines to patients with complex, chronic multimorbidity, but also provide information and advice in a patient-centered way. One way to achieve this is to use motivational interviewing.
As outlined in the Australian Journal of General Practice, “A motivational interviewing conversation is one where the clinician engages with the patient and supports behavioural change through a deliberate focus on the patient’s preferences, needs and values.” This approach has been found to be more effective in promoting behaviour change than simply providing patients with generic advice.
Motivational interviewing may include:
- Reflective statements (e.g. “It sounds as though you are frustrated as you feel you have already tried to lose weight many times in the past.”
- Advice with permission (e.g. “Would it be ok if I provide you with some information about the effects of alcohol on the body?”)
- Purposefully eliciting patient ideas (e.g. “What do you understand about the issues related to having high blood pressure?”)
But to be clear, this approach does NOT entail confrontation, coercion or telling patients what to do!
So how is this relevant to the Clinical Competency Exam (CCE) I hear you ask? It is highly likely that you will come across a patient counselling station where you will be expected to display your skills in this area, as it is core GP business.
Here is our advice on how to upskill in this important area.
Step #1:
Read this key article from the Australian Journal of General Practice (2018)
Step #2:
Practise using the steps outlined in this article with your patients. Here is a recap:
- Engage – Connect with the patient (hint: check out Figure 1 below for some helpful statements you may wish to steal!)
- Focus – Explore options to find a helpful focus. For example, “You seem to have concerns about your health. What is the most important thing that you wish to focus on now?” If the patient is struggling to answer, you can ask “Is it ok if I suggest a starting point that might be helpful?” Ask the patient to rate the importance of the behaviour change and their confidence in making that change from 0 to 10.
- Evoke – Listen for reasons, preferences, strengths and values. The secret here is to use open questions, for example, “Why is not drinking alcohol important to you?” “Tell me some of the reasons you have considered quitting smoking?” “What are some of the things that you think you might be able to do to improve your mood?” “How do you think you could build on the sleep strategies you have already started using?”
- Plan – Make a plan together – note the last word here…together. The focus of this approach is to remain patient-centred
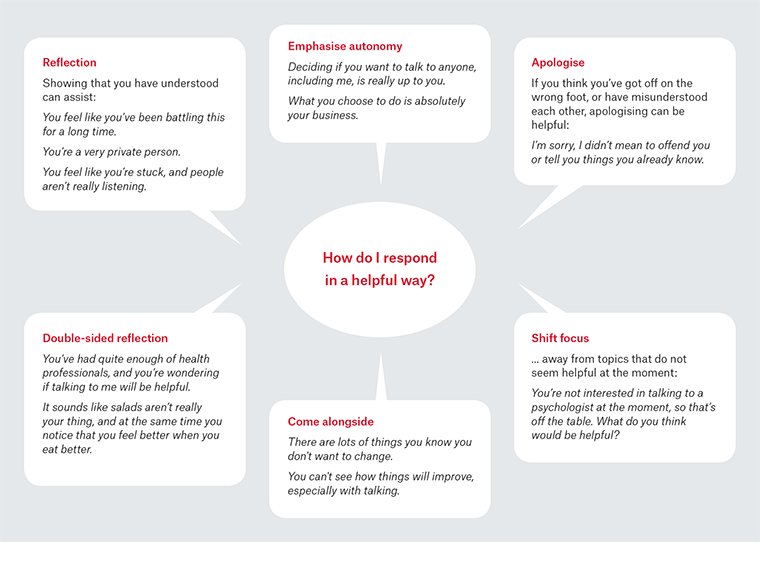
AJGP: Figure 1: Helpful responses to engage, respond to arguments against making changes, and to diffuse discord
Step #3:
Reflect on how your skills are developing over time. How confident do you feel with using motivational interviewing? Do you have any tips for promoting behaviour change which have worked really well with your patients? Feel free to share them with us!
As you have probably gathered by now, simply having knowledge of motivational interviewing conversations and the framework described here isn’t adequate. You need to practice using this skill in your everyday clinical practice so that it becomes second nature. And of course, you will then do this without thinking in the CCE! If you feel you would benefit from additional support for preparing for your upcoming CCE, please contact us at GPEx so that we can find a program to suit your needs.
Reference:
McKenzie KJ, Pierce D, Gunn JM. Guiding patients through complexity: Motivational interviewing for patients with multimorbidity. Australian Journal of General Practice 2018; 47 (1-2). https://www1.racgp.org.au/ajgp/2018/january-february/guiding-patients-through-complexity-(1)